In the fourth year of the pandemic, long COVID is emerging as a major public health concern. However, the medical community is yet to arrive at a clear understanding of what the condition is, what causes it, and how to treat it.
“Long COVID is at the forefront of everyone’s mind,” says Dr Joe Kosterich, a Perth-based GP. He’s not wrong. Long COVID is a serious public health concern – on this, Australia’s political class, public health experts, and health professionals are largely in agreement.
The problem, says Dr Kosterich, is that the medical community is yet to determine exactly what long COVID is, much less how to treat it. “Medicine wants to put labels on conditions,” Dr Kosterich explains. “We’re quite good at giving it a name and recognising patterns, but that doesn’t always tell the why and how to fix it.”

Official estimates suggest that between five to ten per cent of those who have been infected will have long COVID, meaning that as many as 500,000 to one million Australians could now have, or have had the condition. But what, exactly, does that mean?
The World Health Organisation (WHO) defines long COVID as, “the continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least 2 months with no other explanation.” If that sounds broad, that’s because the definition encompasses more than 200 different symptoms involving multiple systems and organs. The National Clinical Evidence COVID-19 taskforce definition of long COVID dispenses with the caveat that symptoms must last two months, inching the diagnostic net that little bit wider.
“In the simplest terms, if you catch COVID, still feel unwell several months later, and your symptoms can’t be attributed to any other cause, you can be diagnosed with long COVID,” says Dr Kosterich.
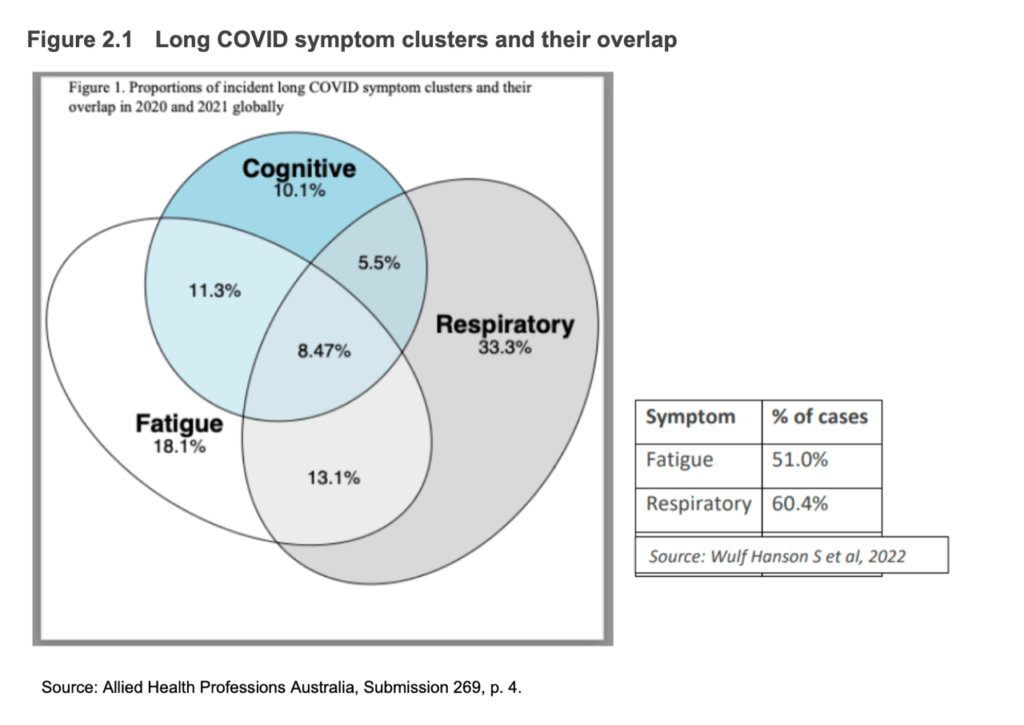
An exhaustive review published in Nature earlier this year summarises much of what we know from two years of research into long COVID. The condition affects multiple organ systems, with symptoms including fatigue, shortness of breath, cognitive dysfunction, depression, headaches, gastrointestinal upset, skin rashes, and more. Long COVID symptoms can vary widely in severity, from mild, to life-altering, and women are more likely to experience long COVID symptoms than men.
Yet, there is conflicting scientific evidence on whether long COVID is a unique condition compared to other post-viral syndromes, or whether it is necessarily associated with COVID infection.

“Many viruses can cause long term symptoms,” says Dr Kosterich, citing Ross River virus, glandular fever and cytomegalovirus (CMV) as examples. The question is, how much more prevalent and severe is long COVID compared to other long-viral syndromes? Maybe not very much, according to a new study by Queensland Health. Researchers comparing prevalence and severity of long symptoms post-COVID and post-influenza in the Queensland population found no significant difference between the two groups.
Similarly, a US study of 1,000 adults with symptomatic illness found that at the three month follow up, the non-COVID infected group had higher prevalence of long COVID symptoms (53.5%) than the infected group (39.6%). This finding was suggestive that while many people who have been infected with COVID experience ongoing symptoms, other factors, including prior illness with other respiratory viruses, may also contribute to long symptoms.
Expanding on those ‘other factors’, as early as 2021, a French study of nearly 27,000 adults made the surprising finding that prior infection with COVID was not associated with long COVID symptoms at all. Even more surprising was the finding that belief of a prior infection was associated with long COVID symptoms. The researchers were able to separate our belief of infection from actual infection by comparing self-reported infections to antibody tests from surveyed participants.
Likewise, a more recent study found no link between long COVID and prior COVID infection. Researchers followed a group of young Norwegians (aged 12 to 25 years) for six months, comparing individuals who had mild or moderate COVID infections (non-hospitalised) to a control group who had never been infected. At the end of the six months, both groups had approximately the same prevalence of long COVID symptoms (48.5% in the COVID–positive group and 47.1% in the control group). Symptom prevalence correlated with loneliness and poor physical activity. Participants who experienced more severe symptoms at baseline, irrespective of COVID infection, were also more likely to have persistent symptoms six months later.
Then there is ‘long mask’, or Mask-Induced Exhaustion Syndrome (MIES). A systematic review of studies assessing adverse medical mask effects (surgical and N95) found that prolonged mask wearing significantly restricted oxygen intake and hindered carbon dioxide release, both of which produce symptoms overlapping with the WHO case definition of long COVID.
These studies highlight the difficulty that doctors face in diagnosing non-specific post-infection symptoms. “Myalgias, fatigue, brain fog – these kinds of symptoms overlap with other conditions, and without a diagnostic test for long COVID, teasing out one condition from another can be challenging,” says Dr Kosterich.
Given this symptom overlap, and in the context of a culture of censorship in the Australian medical profession, there is the possibility that some vaccine adverse events will be diagnosed as long COVID. “Vaccine injury is a subject that few in the medical profession have wanted to talk about,” Dr Phelps states in her submission. Dr Kosterich agrees that “doctors don’t want to appear anti-vax.” It is also very time consuming for doctors to reporting adverse events, a task for which doctors are not paid.
The issue of symptom overlap is raised in several submissions to the federal Long COVID Inquiry. “There is a significant overlap in the range of symptoms seen in Long Covid and the serious ongoing symptoms caused by COVID-19 vaccine adverse reactions,” states COVERSE, Australia’s leading support network for the COVID vaccine injured, in their submission (#516). Former president of the Australian Medical Association (AMA), Dr Kerryn Phelps, who is herself COVID vaccine injured, itemises many of the overlapping symptoms in her own submission (#510).
This must trigger a change of tack by governments to limit increase of LC case numbers by prevention measures https://t.co/XwXkeb8v8J
— Prof Kerryn Phelps AM (@drkerrynphelps) April 25, 2023
Have we been able to give informed consent for covid vaccines when we have not been informed of the known risks?
— Kara Potter (@KaraPotter26273) April 17, 2023
I willingly supported the government in the vaccine rollout. I believed them. I had 3 shots. It has changed my life forever. #believeus #canwetalkaboutit pic.twitter.com/1ndE56f2NB
When asked about his opinion on the conflicting science on the issue of long COVID, Dr Kosterich remarks that, while medical science has been presented in recent times as a black and white discipline, historically it has been anything but. “It’s the nature of medical studies to be conflicting,” he says. “Medicine exists in a world of uncertainty.”
“What doctors need to focus on now is, as best possible, relieving symptoms,” says Dr Kosterich, pointing out that allopathic medicine is very good at the symptom-relief approach. Lifestyle changes should not be underestimated either, he adds. “Metabolic health is a primary determinant of COVID outcomes. Exercise, adequate Vitamin D, these are simple things people can do to improve their health.” Dr Kosterich’s integrative approach is in line with long COVID management guidelines from the Royal Australian College of General Practitioners (RACGP), which recommend “a holistic, person-centred” approach involving assessment of physical, cognitive, psychological and psychiatric symptoms, as well as functional abilities.
Further research into long COVID will be of great benefit to doctors, who rely on published research to inform diagnosis and treatment on the ground. A new $6.4 million grant awarded to Griffith University for research into the potential overlap between long COVID myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is example of the kind of research that is needed in this area. On Monday, the Federal Government announced a further $50 million to be dedicated to research into long COVID.



